- Augusta University
- Centers & Institutes
- Vascular Biology Center
- Gábor Csányi - Research & Publications
Gábor Csányi - Research & Publications
← Back to main
Research Description
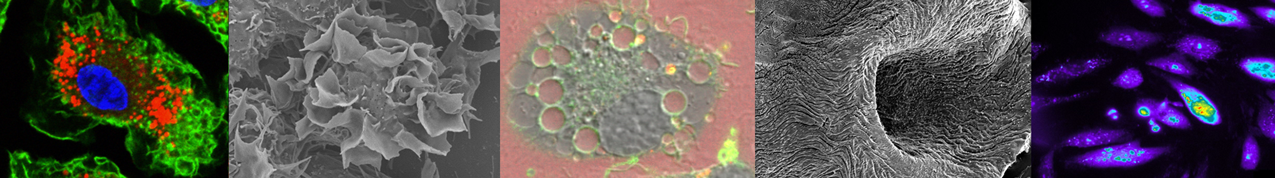
Our laboratory employs transgenic and knockout mouse models, lineage tracing, isolated human cardiac and vascular tissue, fluorescent and high-resolution imaging techniques, RNA-seq, spatial transcriptomics, and a wide variety of other molecular and biochemical tools to better understand how arterial and venous diseases develop. A major area of focus in the laboratory is to determine the signaling mechanisms regulating macropinocytosis and its role in cardiovascular and other pathologies. We developed a number of animal models, imaging techniques and novel pharmacological and genetic approaches to better understand how this unique endocytic process participates in cardiovascular diseases. Our experiments are conducted in close collaboration with physician-scientists and involve an integrative approach consisting of a wide range of physiological, pharmacological and molecular tools, human cells and tissue and genetically engineered mouse models.
1. To investigate the role of macropinocytosis in macrophage foam cell formation in
atherosclerotic arteries.
2. To determine the role of LDL macropinocytosis in phenotypic modulation of vascular
smooth muscle cells in atherosclerotic arteries.
3. To examine exosome-mediated intercellular communication between endothelial cells
and neutrophils in the development of abdominal aortic aneurysms.
4. To study the mechanisms by which matricellular proteins regulate lymphangiogenesis.
5. To investigate venous smooth muscle cell reprogramming in cardiovascular diseases.
Spotlight Publications
1. Lin H, Singla B, Ghoshal P, Ahn W, Ghoshal P, Blahove M, Cherian-Shaw M, Chen A, Haller A, Hui DY, Dong K, Zhou J, White J, Stranahan AM, Jasztal A, Lucas R, Fulton D, Stansfield BK, Chlopicki S and Csányi G. Receptor-independent fluid-phase macropinocytosis promotes arterial foam cell formation and atherosclerosis. Sci Transl Med. 2022, 14(663):eadd2376. PMID: 36130017.
Highlighted in Nature Reviews Cardiology; PMID: 36195684.
2. Singla B, Lin H, Ahn W, Xu J, Ma Q, Sghayyer M, Dong K, Cherian-Shaw M, Zhou J, Huo Y, White J, and Csányi G. Loss of myeloid cell-specific SIRPα, but not CD47, attenuates inflammation and suppresses atherosclerosis. CardiovasC Res. 2021; PMID: 34940829.
3. Singla B, Lin H, Chen A, Ahn W, Ghoshal P, Cherian-Shaw M, White J, Stansfield BK, and Csányi G. Role of R-spondin 2 in arterial lymphangiogenesis and atherosclerosis. CardiovasC Res. 2021; 117:1489-1509. PMID: 32750106.
Highlighted in CardiovasC Res; PMID: 33712820.
4. Ghoshal P, Singla B, Lin H, Cherian-Shaw M, Tritz R, Padgett CA, Hudson F, Zhang H, Stansfield BK, and Csányi G. Loss of GTPase activating protein neurofibromin stimulates paracrine cell communication via macropinocytosis. Redox Biology. 2019; 101224. PMID: 31201114.
5. Lin HP, Ghoshal P, Singla B, Faulkner JL, Shaw M, O’Connor PM, She X, Belin de Chantemele E, Csányi G. Identification of novel macropinocytosis inhibitors using a rational screen of FDA-approved drugs. British Journal of Pharmacology. 2018, 175:3640-3655. PMID: 29953580. PMCID: PMC6109223
6. Ghoshal P, Singla B, Lin H, Feck DM, Cantu-Medellin N, Kelley EE, Haigh S, Fulton D, and Csányi G. Nox2-Mediated PI3K and Cofilin Activation Confers Alternate Redox Control of Macrophage Pinocytosis. Antioxid Redox Signal. 2017; 26:902-916. PMID: 27488058. PMCID: PMC5455614.
Highlighted in Antioxid Redox Signal; PMID: 28288516.
Cover image: