October 2025
35 Year-old Female Slumped in Her Chair 15 Minutes Ago
Author: Manpreet Luthra MD PGY-3
Peer Reviewers: Lee LaRavia, DO; Dan Kaminstein, MD
Christopher Crawley, MD; Vijay Reddy, MD
Learning Objectives:
- Using US as a diagnostic tool and as a guide to medical resuscitation in the patient with syncope.
- Demonstrate the importance of re-evaluation of patient with US after an acute change
- Discuss the US charactereistics/findings pertinent to Massive and Submassive PE
- Review ultrasound specificities and sensitivities specif to PE
- Highlight the early pressor support is more beneficial in submassive and massive PE than aggressive IV fluids
Case Presentation
-
Intellectually disabled and deaf 35 yo F here for reported syncopal episode that lasted
a few minutes while seated at dinner (approximately 15 minutes ago). Currently at
baseline. At the time, her deaf boyfriend was with her but not with her at presentation.
Patient is accompanied by boyfriend’s grandmother. She states that she had some
chest pain just before the episode. -
HR:104, BP:98/56, RR: 20, SpO2: 98%, T: 97.6F, BG 145.
-
PE: Currently at baseline. Mild bilateral CVA tenderness
-
Labs and Imaging: Blood Culture x 2, POC Preg, EKG 12 lead, BG,UA w/ Culture,
Lactic acid, BNP, CBC, CMP, CK, Lipase, POC troponin, Ethanol , Acetaminophen,
Salicylate, UDS, TSH, T4, CTA Chest PE, CT Abdomen Pelvis w/contrast, Chest XR
2 View -
DDX: Hypoglycemia, Myocardial Infarction, Seizure, Congenital/premature aortic
stenosis, Electrolyte imbalance, Sepsis/Septic shock 2/2 pyelonephritis?, Arrythmia,
Pulmonary Embolism, Stroke, Toxin, Head trauma
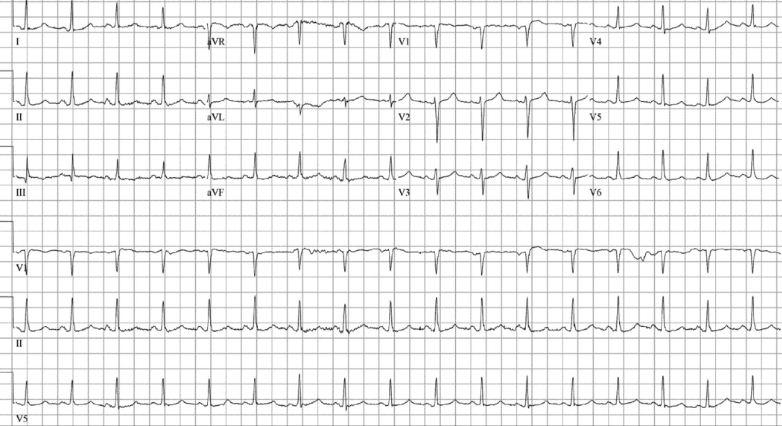
ECG and Initial Labs
- POC Troponin: 0.0
Initial POCUS Images
- Plax View
- Short Axis View
15 minutes Later
Patient goes to the bathroom. Has a syncopal event in the restroom. Remains tachycardic with BP of 70’/50’s. Hypoxic to the 70’s. Placed on NIV but did not tolerate > High Flow. Started on Levophed. Rushedto CT, but before she did…
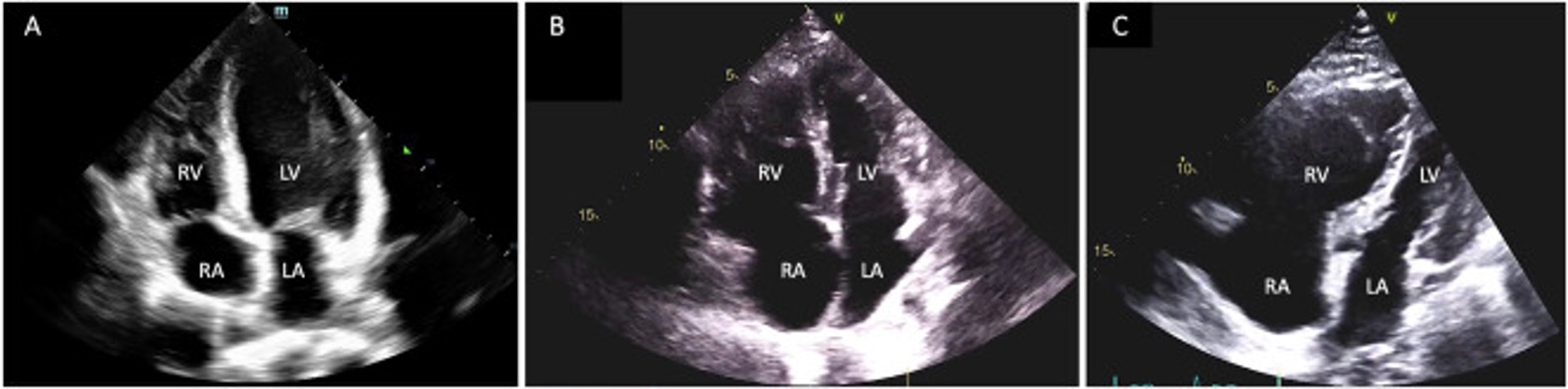
Re-assessment POCUS
- Apical View
- Short Axis
- Plax View
CTA CHEST (Radiology Read: Patient already in the CVICU)
-
Severe interval worsening of pulmonary emboli clot burden, now involving the bilateral main pulmonary arteries, with occlusive pulmonary emboli in the right upper, middle and lower lobes and left lower lobe. Nonocclusive pulmonary emboli in the left upper lobe.
-
Imaging findings of severe right heart strain with bowing of the interventricular septum into the left ventricle, and severely elevated RV/LV ratio of 2.0. Backing of intravenous contrast into the liver veins as well. Emergent PERT consultation is recommended.
Diagnosis and Case Disposition
- Diagnosis: Massive PE
- Labs return showing severe lactic acidosis. BNP: 240’s
- Patient is maxed on Levophed and continues to decompensate. Considering
central line and adding vasopressin. - Decided to use TPA with pharmacy’s help.
- Patient was stable on current pressor requirements. CT Surgery attending
agrees to take the patient for thrombectomy. - Patient does well and is discharged from CVICU with IVC filter and long-term
anticoagulation.
Pulmonary Embolism Severity Stratification
-
American Heart Association and European Society of Cardiology have agreed to three classifications of pulmonary embolism
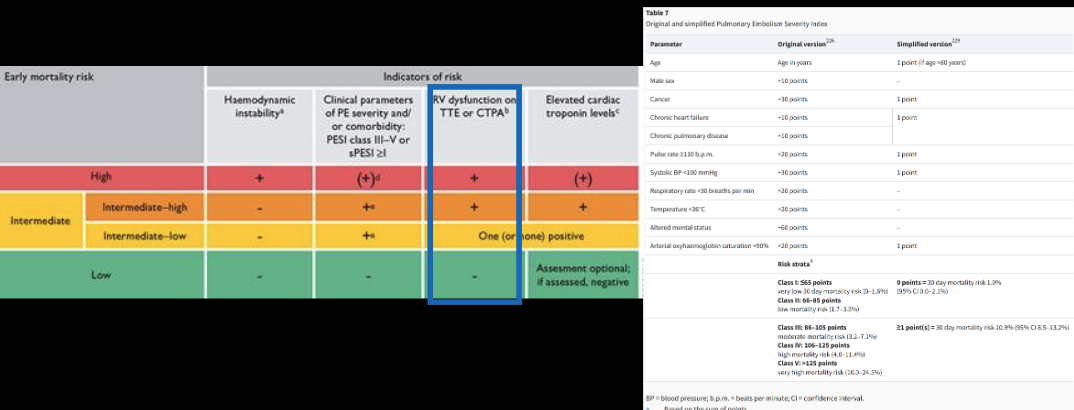
Severity Ultrasound Findings that Suggest PE
- There are numerous findings that can assist yu in identifying and classifying a PE
on US
- 1. RV:LV ratio (Sensitivity 46%, Specificity 91%)
2. Abnormal septal wall motion (Sensitivity 28%, Specificity 95%)
3. McConnel’s sign (Sensitivity 19%, Specificity 98%)*
4. Tricuspid Regurgitation Velocity (Sensitivity 46%, Specificity 87%)
5. Elevated pulmonary artery systolic pressure (Sensitivity 65%, Specificity 74%)
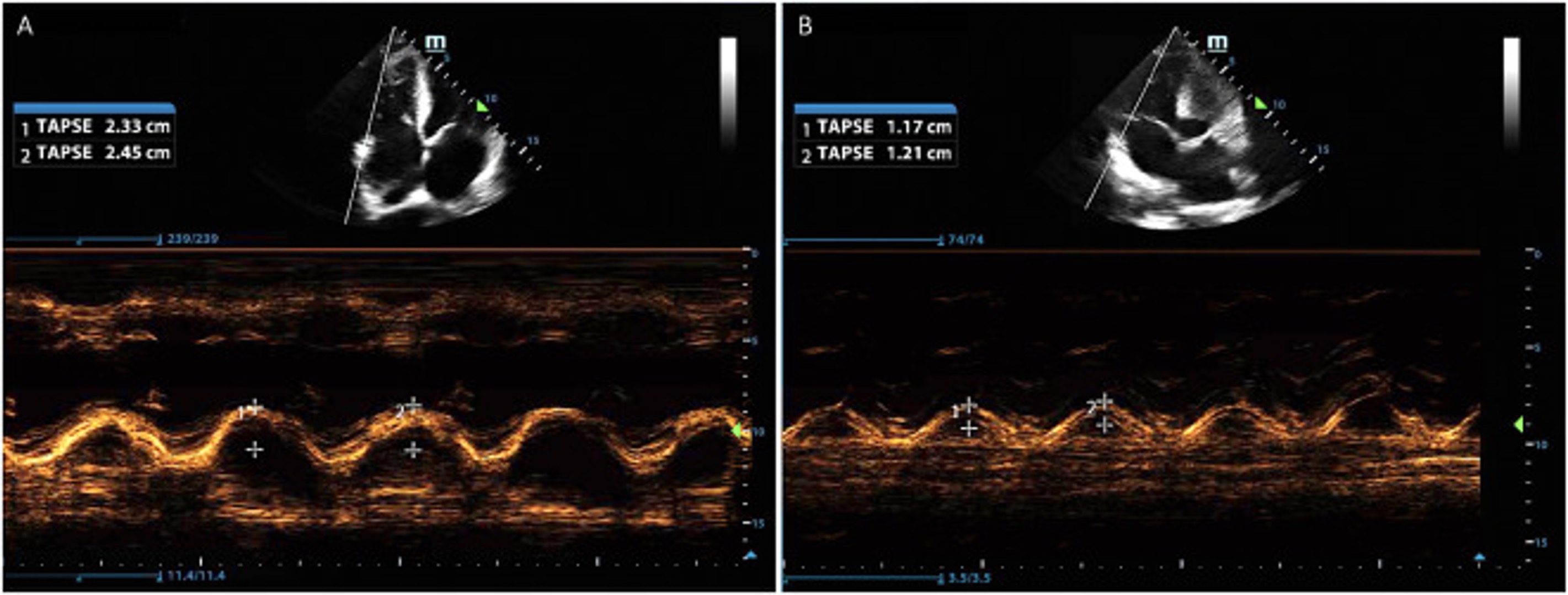
6. Decreased tricuspid annular plane systolic excursion (TAPSE) (Sensitivity 66%, Specificity 88%) *
7. Decreased S’ (Sensitivity 82-83%, specificity 68-86%)*
8. Pulmonary artery mid-systolic notching (Sensitivity 92%, Specificity 99%)*
- 1. RV:LV ratio (Sensitivity 46%, Specificity 91%)
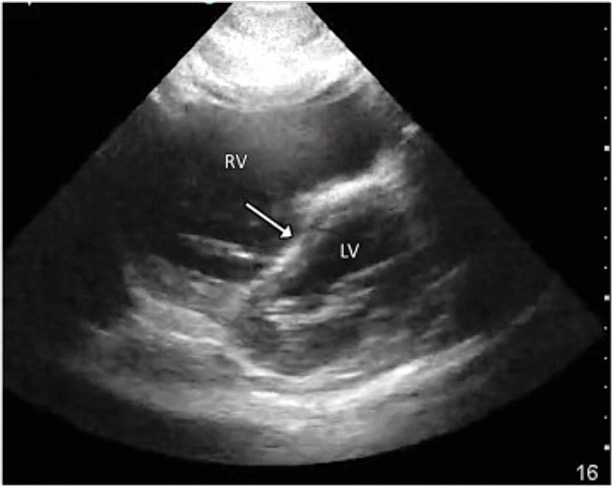
Ultrasound Findings that Suggest PE
-
RV:LV ratio: Normal is .67:1, mild dilation is .67:1 to 1:1, moderate dilation is 1:1 to 1.5:1, and severe dilation is greater than 1.5:1
-
Septal Flattening (“D sign”)
-
McConnell Sign
-
Tricuspid Annular Plane Systolic Excursion (TAPSE) < 17mm / 1.6cm => RV systolic dysfunction. Normal mean is 24mm +/- 3mm.
- Normal Abnormal
Take Away Points
-
Re-assess patients after an acute change, going through the ABC's with US.
-
LV hyperdynamic collapse does not necessarily mean the patient needs IV
fluids.-
In submassive and massive PE, IV fluids can worsen right ventricular strain and potentially reduce cardiac output, particularly in the presence of right ventricular dysfunction.
-
Early pressor support is more beneficial than aggressive IV fluids
-
- There are a few rapid and easy US assessment tools and findings that can
help evaluate and risk stratify PE and change management.
References
1. Afonso, L., Sood, A., Akintoye, E., Gorcsan, J., Rehman, M. U., Kumar, K., Javed,
A., Kottam, A., Cardozo, S., Singh, M., Palla, M., Ando, T.,
Adegbala, O., Shokr, M., & Briasoulis, A. (2019). A Doppler Echocardiographic Pulmonary
Flow Marker of Massive or Submassive Acute
Pulmonary Embolus. Journal of the American Society of Echocardiography, 32(7), 799–806.
https://doi.org/10.1016/j.echo.2019.03.004
2. Alerhand, S., Sundaram, T., & Gottlieb, M. (2021). What are the echocardiographic
findings of acute right ventricular strain that suggest
pulmonary embolism? Anaesthesia, Critical Care & Pain Medicine, 40(2), 100852. https://doi.org/10.1016/j.accpm.2021.100852
3. Daley, J. I., Dwyer, K. H., Grunwald, Z., Shaw, D. L., Stone, M. B., Schick, A.,
Vrablik, M., Kennedy Hall, M., Hall, J., Liteplo, A. S., Haney, R.
M., Hun, N., Liu, R., & Moore, C. L. (2019). Increased Sensitivity of Focused Cardiac
Ultrasound for Pulmonary Embolism in Emergency
Department Patients With Abnormal Vital Signs. Academic Emergency Medicine, 26(11),
1211–1220. https://doi.org/10.1111/acem.13774
4. Fields, J. M., Davis, J., Girson, L., Au, A., Potts, J., Morgan, C. J., Vetter,
I., & Riesenberg, L. A. (2017). Transthoracic Echocardiography for
Diagnosing Pulmonary Embolism: A Systematic Review and Meta-Analysis. Journal of the
American Society of Echocardiography, 30(7), 714-723.e4. https://doi.org/10.1016/j.echo.2017.03.004
5. Konstantinides, S. V., Meyer, G., Becattini, C., Bueno, H., Geersing, G.-J., Harjola,
V.-P., Huisman, M. V., Humbert, M., Jennings, C. S.,
Jiménez, D., Kucher, N., Lang, I. M., Lankeit, M., Lorusso, R., Mazzolai, L., Meneveau,
N., Ní Áinle, F., Prandoni, P., Pruszczyk, P., & Righini,
M. (2019). 2019 ESC guidelines for the diagnosis and management of acute pulmonary
embolism developed in collaboration with the europeanrespiratory society (ERS). European
Heart Journal, 41(4), 543–603. https://doi.org/10.1093/eurheartj/ehz405
6. POCUS in Practice. (2022a, January 11). How to... Measure TAPSE. YouTube. https://www.youtube.com/watch?v=DmRotfyMIQw
7. POCUS in Practice. (2022b, January 11). How to... Measure TV s’. YouTube. https://www.youtube.com/watch?v=fY4iiYvBC2Q
8. Wahl, A., Praz, F., Schwerzmann, M., Bonel, H., Koestner, S. C., Hullin, R., Schmid,
J.-P., Stuber, T., Delacrétaz, E., Hess, O. M., Meier, B., & Seiler, C. (2010). Assessment
of right ventricular systolic function: Comparison between cardiac magnetic resonance
derived ejection fraction and pulsed-wave tissue Doppler imaging of the tricuspid
annulus. International Journal of Cardiology, 151(1), 58–62.
https://doi.org/10.1016/j.ijcard.2010.04.089