The Cui Lab
Yan Cui, PhD
Professor, Biochemistry & Molecular Biology
Professor, Graduate Studies
Member, Cancer Immunology, Inflammation and Immunotherapy Program
Jump to: Research Summary Research Interests Selected Publications Research Team
Contact Us
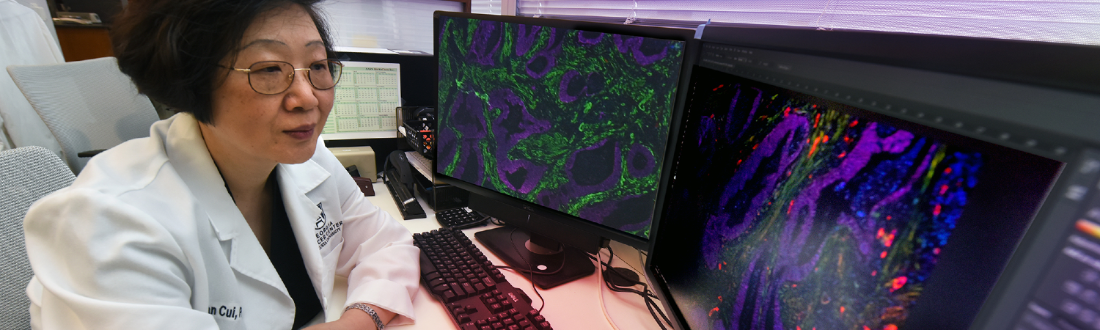
The Yan Cui Lab
Health Sciences Campus
GCC - M. Bert Storey Research Building
1410 Laney Walker Blvd., CN-4133A3
(706) 723-4153
Research Summary
The major research interest of the Cui lab is focused on understanding the cellular and molecular mechanisms by which tumor-host interactions dictate the immunological landscape of the tumor microenvironment (TME), and developing novel translatable strategies to improve therapeutic outcome via targeting the tumor-host communications. Specifically, we are actively pursuing in the areas described below.
Research Interests
The CD73-adenosinergic signaling as a critical immune checkpoint and therapeutic target during tumor progression and treatment
CD73 (ecto-5'-nucleotidase) is a cell surface molecule that regulates tissue homeostasis and immune response via producing extracellular adenosine (eADO). In the tumor microenvironment (TME) during tumor progression and cancer therapy, the CD73-adenosinergic signaling is further exacerbated by hypoxia, cellular stress, injury, and apoptosis. Therefore, CD73 is a detrimental metabolic and immune checkpoint that promotes immunosuppression, tumor progression and metastasis. Compelling evidence demonstrates that CD73 levels in the TME of many tumor types, including colorectal cancer (CRC) and head and neck squamous cell carcinoma (HNSC), are highly elevated and their increased CD73-adenosinergic activity is linked to poor patient survival. Mechanistically, the immunosuppressive and pro-tumor effects of CD73-ADO are primarily mediated through activation of A2A and/or A2B receptors on cells located in close proximity to CD73-positive cells. Thus, targeting the CD73-ADO pathway during tumor progression and treatment represents an attainable strategy to improve therapeutic outcomes. Employing the advanced artificial-intelligence (AI)-assisted spatial analysis technology with clinical specimens and pre-clinical models, we aim to define the specific cell types and adenosinergic pathways in spatial context that are actively suppressing antitumor immunity during tumor progression and therapy. The overarching goal is to develop effective CD73-adenosinergic immune checkpoint blockade regimens for improving therapeutic outcomes.
The role of cancer associate fibroblasts in dictating the immunosuppressive landscape of the TME
Cancer associated fibroblasts (CAFs) are specialized fibroblastic stroma in the complexed TME, which play crucial roles in shaping the immune landscape of the TME. CAFs are highly potent promoters of cell survival, proliferation, angiogenesis, extracellular matrix (ECM) remodeling and immunosuppression, all of which contribute to their pivotal roles in supporting tumorigenesis, tumor progression, chemoresistance and metastasis. Clinically, high CAF abundancy in the TME of many tumor types is associated with more aggressive tumor progression and poor clinical prognosis. Recent advances in our understanding of fibroblast biology demonstrate that CAFs are highly heterogeneous and plastic in phenotype and function, revealed as the coexistence of various distinct CAF subtypes in the TME. Correspondingly, it has been shown in a few different tumor types that some CAFs manifest pro-tumor while others anti-tumor properties. It is not well understood how the fibroblast/CAF phenotype and function are modulated by environmental factors in a tissue/tumor-specific, tumor progression, or treatment-dependent manner and vice versa. Recent studies in our laboratory employing preclinical models and clinical specimens demonstrate that CAFs exploit many of the known immunosuppressive mechanisms of the host for tissue homeostasis, such as COX2-PGE2 axis, CD73-eADO pathway, and the PD-L1 checkpoint, to exacerbate immune tolerance in the TME. We are actively investigating the crucial cellular and molecular mechanisms that underscore the immunosuppressive capacity of CAFs through their interaction with neighboring myeloid derived suppressor cells, T cells and tumors. Better understanding of the immunosuppressive function of CAFs in dictating the immune landscape of the TME will provide invaluable information for new strategies to target specific aspects of CAF to improve immunotherapy efficacy and clinical outcome.
The immunoregulatory effects ofp53dysfunction in tumorigenesis and progression for targeting the p53 pathway in the TME to improve immunotherapy outcomes
The tumor suppressor p53 (Trp53), a frequently mutated/inactivated gene in tumors, is the most frequently mutated gene in HNSC related to tobacco and alcohol consumption. Trp53 suppresses tumor development by inducing apoptosis or senescence, which is a major mechanism of tumor suppression of p53. Compelling evidence suggests that p53 also suppresses tumorigenesis by regulating other crucial biological functions, including host immune responses. As chronic inflammation plays a vital role in tumor initiation, progression, and metastasis, it is plausible that p53 inactivation/dysfunction promotes tumorigenesis and tumor progression by compromising host immune surveillance and altering tumor milieu to pro-tumor inflammation. Our studies demonstrated in preclinical models that p53 inactivation in the TME skews the immunological landscape toward pro-inflammation and pro-tumor progression through alternating the ratio of immunosuppressive vs immunostimulatory myeloid cell populations via direct or indirect mechanisms. Furthermore, we also demonstrate that targeted activation of the p53 pathway in the TME promotes antitumor immunity and improves tumor-free survival. We are exploring new strategies of repurposing and/or expanding the application of pharmacological and biological p53 activation/reactivation in tumor and myeloid cells together with PD-1/PD-L1 or CD73-adenosinergic checkpoint blockade for tumor treatment that elicits synergistic effects of tumoricidal and antitumor immunity to maximize antitumor efficacy for tumors maintaining wild-type p53 as well as those that incur p53 mutations.
Selected Publications
Inhibitors of the CD73-adenosinergic checkpoint as promising combinatory agents for
conventional and advanced cancer immunotherapy
Kurago, Z., Guo, G., Shi, H., Bollag, R. J., Groves, M. W., Byrd, J. K. & Cui, Y., 2023, In: Frontiers in immunology. 14, 1212209.
Yu, M, Guo, G, Huang, L, Deng, L, Chang, C, Achyut, BR, Canning, M, Xu, N, Arbab, AS, Bollag, R., Rodriguez, PC, Mellor, A, Shi, H, Munn, D, Cui, Y (2020) CD73 on cancer-associated fibroblasts enhanced by the A2B-mediated feedforward circuit enforces an immune checkpoint. Nat Comms. 11 (1): 515. Doi: 10.1038/s41467-019-14060-x. PMID: 31980601. PMCID: PMC6981126
Canning, M, Guo,G, Yu, M, Myint, C, Groves, MW, Byrd, JK, Cui, Y (2019) Heterogeneity of the Head and Neck Squamous Cell Carcinoma Immune Landscape and Its Impact on Immunotherapy. Front Cell Dev Bio. 7:52. doi: 10.3389/fcell.2019.00052. PMID:31024913. PMC6465325.
Sharma, MD, Rodriguez, PC, Koehn, BH, Baban, B, Cui, Y, Guo, G, Shimoda, M, Pacholczyk, R, Shi, H, Lee, EJ, Xu, H, Johnson, TS, He, Y, Mergoub, T, Venable, C, Bronte, V, Wolchok, JD, Blazar, BR, Munn, DH. (2018) Activation of p53 in Immature Myeloid Precursor Cells Controls Differentiation into Ly6c+CD103+Monocytic Antigen-Presenting Cells in Tumors. Immunity. 16;48(1):91-106.e6. doi: 10.1016/j.immuni.2017.12.014. PMID:29343444.
Guo, G., Yu, M., Xiao, W., Celis, E., Cui, Y. (2017) Local activation of p53 in the tumor microenvironment overcomes immune suppression and enhances antitumor immunity. Cancer Res. 77(9); 2292–2305. doi: 10.1158/0008-5472.CAN-16-2832. PMID: 28280037; PMCID: PMC5465961.
Yu, M., Guo, G., Zhang, X., Li, L., Yang, W., Bollag, R., Cui, Y. (2017) Fibroblastic reticular cells of the lymphoid tissues modulate T cell activation threshold during homeostasis via hyperactive cyclooxygenase-2/prostaglandin E2 axis. Sci. Rep. 7:3350, DOI:10.1038/s41598-017-03459-5; PMID: 28611431.
Guo, G., Marrero, L., Rodriguez, P., Del Valle, L., Ochoa, A., Cui, Y. (2013) Trp53 inactivation in the tumor microenvironment promotes tumor progression by expanding the immunosuppressive lymphoid-like stromal network. Cancer Res. 73(6):1668-75. PMID: 23319800. PMCID: PMC3602383. (Priority report, cover story)
Kibe, R., Zhang, S-Z., Guo, D., Marrero, L., Tsien, F., Rodriguez, P., Khan, S., Zieske, A., Huang, J., Li, W., Durum, S.K., Iwakuma, T., Cui, Y. (2012) IL-7R deficiency in p53null mice exacerbates thymocyte telomere erosion and lymphomagenesis. Cell Death Differ. 19(7):1139-51. PMID: 22281704. PMCID: PMC3374079.
Research Team


Reducing the Burden
The Georgia Cancer Center at Augusta University is dedicated to reducing the burden of cancer in Georgia and across the globe through superior care, innovation, and education. Through unprecedented expansion, the Georgia Cancer Center is providing access to more first-in-the-nation clinical trials, world-renowned experts and life-saving options.
Follow the Georgia Cancer Center