Selner's Rhinolaryngoscopy Online

John C. Selner, MD
William K. Dolen, MD
Bryan Spofford, MD
Jerald W. Koepke, MD
Chapter 3. NORMAL ANATOMY OF THE UPPER AIRWAY
|
For convenience in the study of anatomy and pathology, the upper airway may be divided into sections (Figure 1). In adults, the nasal cavity is a channel approximately nine to ten centimeters in length from the meatus to the choana. The choana (posterior naris) separates the nasal cavity from the nasopharynx. The oropharynx, in which the palatine tonsils are located, extends from the inferior margin of the soft palate to the upper edge of the epiglottis. The hypopharynx is located posterior to the aperture of the larynx. The triangular inlet of the larynx (aditus laryngis) is formed by the superior margin of the epiglottis, the aryepiglottic folds, and the arytenoid cartilages. The larynx becomes continuous with the trachea. |
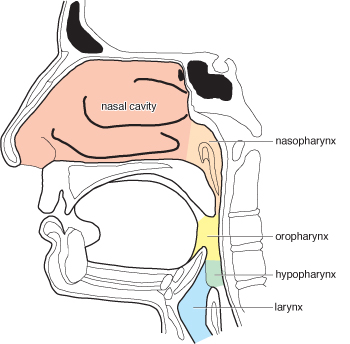 Figure 1. The anatomic divisions of the upper airway. All five divisions may be inspected
with a fiberoptic endoscope. Figure 1. The anatomic divisions of the upper airway. All five divisions may be inspected
with a fiberoptic endoscope. |
ANTERIOR NASAL STRUCTURES
|
The nasal cavity is divided into right and left chambers by the nasal septum, which may deviate considerably from the midline. The nasal vestibule is the most anterior and inferior portion of the nasal cavity (Figure 2). It is bounded medially and laterally by the alar cartilages and extends to the inferior border of the lateral nasal cartilage. The vestibule is lined by skin, rather than by mucosa, which gives rise to the vibrissae, coarse nasal hairs which serve as a protective mechanism. Above the vestibule and in front of the middle meatus is the nasal atrium, and above this is the agger nasi, a prominence which generally contains anterior ethmoid air cells. The nasal valve is located at the junction of the vestibule and the nasal vault. This structure, whose cross sectional area is regulated by the dilator naris muscle, provides substantial resistance to air flow. The nasal floor is formed anteriorly by the maxillary bone and posteriorly by the palatine bone. It is slightly concave and passes horizontally from the vestibule to the choana. The incisive canal is located on the anteromedial nasal floor. The nasal vault narrows superiorly to form the roof of the nose. The middle. portion of the nasal roof is approximately parallel to the nasal floor, but the anterior and posterior parts slope inferiorly. |
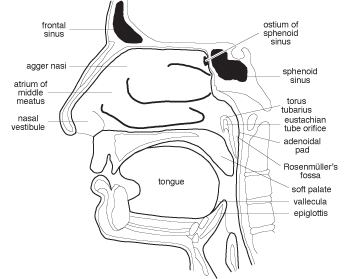 Figure 2. A sagittal section of the head demonstrating lateral structures of the nasal
cavity and pharynx. Figure 2. A sagittal section of the head demonstrating lateral structures of the nasal
cavity and pharynx. |
NASAL SEPTUM
|
The nasal septum consists of both cartilaginous and bony components (Figure 3), with mucous membrane overlying perichondrium or periosteum of the underlying cartilage or bone. The mobile, anterior portion of the septum is composed of a quadrangular septal cartilage resting in a groove on the maxillary bone and articulating posteriorly with the thin, delicate bone of the perpendicular plate of the ethmoid and inferiorly with the thicker, more rigid bone of the vomer. The vomer forms the medial border of the choanae and rests on the crest of the maxillary bone anteriorly and the crest of the palatine bone posteriorly. The perpendicular plate of the ethmoid extends superiorly, attaching to the cribriform plate (lamina cribosa). A superior projection of the hard palate, the maxillary ridge (crista nasalis maxillae; nasal crest of maxilla) often forms a "T" anteriorly at the base of the septum. The lateral wings of the "T" may project into the nasal cavity. The septum is rarely straight in normal adults. A blow to the tip of the nose will cause telescoping, dislocation, or other types of distortion of these delicate bones and cartilages without external signs of a fractured nose. Trauma may result in a septal hematoma with separation of mucoperichondrium from the septal cartilage, resulting in a septal abscess and subsequent perforation. Other injuries may result in chronic nasal obstruction, abnormal nasal function, and change in voice quality. |
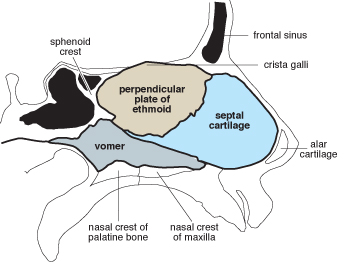 Figure 3. Cartilaginous and bony structures of the nasal septum. The quadrangular
septal cartilage and the vomer articulate with bones of the nasal floor. The thin
perpendicular plate of the ethmoid extends upward to the cribriform plate. Figure 3. Cartilaginous and bony structures of the nasal septum. The quadrangular
septal cartilage and the vomer articulate with bones of the nasal floor. The thin
perpendicular plate of the ethmoid extends upward to the cribriform plate. |
TURBINATES
Three or four turbinates provide filtration, heating and cooling, and humidification of inspired air and offer resistance to air flow. The turbinates are comprised of a scroll shaped bony supporting structure, called a concha, and overlying mucosa. Clefting, or segmentalization, of the turbinates may occur both horizontally and sagittally, and clefting of a middle turbinate may be difficult to distinguish from a nasal polyp on anterior examination. The space created by a turbinate and the lateral wall of the nose is called a meatus.
Inferior Turbinate and Inferior Meatus
|
The inferior concha is a separate bone sitting in an opening in the maxilla and resting in the lateral wall of the nasal passage. It is attached to the palate and maxilla by membranous soft tissue. The turbinate follows the lower lateral wall of the nose in a course parallel to that of the nasal floor. In patients with deviation of the septum, the inferior turbinates are not the same size. The inferior meatus is a convenient passage for advancement of the rhinoscope to the nasopharynx. The only structure opening into the inferior meatus is the nasolacrimal duct which drains tears through a large opening in the anterior roof of the meatus (Figure 4), located about 1 cm. from the anterior margin of the turbinate. Compromise of the nasolacrymal duct can lead to disruption of nasolacrymal drainage and acute and chronic dacryocystitis. The orifice is almost never seen by fiberoptic rhinoscopy. An opening found in. the lateral wall at this location is most likely an antral window surgically placed in the inferior meatus to provide drainage for the maxillary sinus (Figure 6). It is frequently possible to pass the fiberoptic rhinoscope through an antral window in order to assess the status of the maxillary sinus mucosae. |
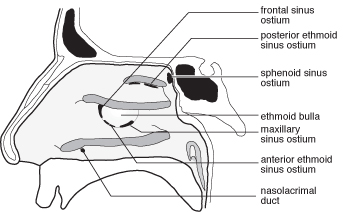 Figure 4. A sagittal section of the head with the turbinates removed to demonstrate
ostia of the paranasal sinuses and nasolacrymal duct. Figure 4. A sagittal section of the head with the turbinates removed to demonstrate
ostia of the paranasal sinuses and nasolacrymal duct. |
Middle Turbinate and Middle Meatus
The middle turbinate, like the superior turbinate, is part of the ethmoid bone and is suspended from the roof of the nose rather than from the lateral wall. The anterior edge is superior and posterior to that of the inferior turbinate.
A crescent shaped cleft, the semilunar hiatus (hiatus semilunaris), is located in the middle meatus (Figure 4). The ostium of the nasofrontaI duct and the anterior ethmoid ostia typically are located in the anterior and midportions of the hiatus. Not infrequently, the nasofrontal duct will have a separate opening anterior to the semilunar hiatus. The maxillary sinuses open into the posteroinferior portion of the hiatus. The ostium of the maxillary sinus varies in size in normals from pinpoint to several millimeters in diameter and large accessory ostia may be present; it is often possible to advance the fiberoptic rhinoscope into the maxillary sinus itself in a patient with a large ostium or a large accessory ostium. Posterior and superior to the semilunar hiatus is the ethmoid bulla (bulla ethmoidalis), a bulge containing anterior and middle ethmoid air cells.
Superior and Supreme Turbinates
The superior turbinate is a short, oblique structure located superior and posterior to the middle turbinate. The posterior ethmoid sinuses drain into the superior meatus (Figure 4). A supreme turbinate medial to the superior turbinate is occasionally noted.
SPHENOETHMOIDAL RECESS
The sphenoethmoidal recess is a deep groove located superior, posterior, and medial to the superior turbinate. It contains the ostium of the sphenoid sinus (Figure 4).
NASOPHARYNX
The torus tubarius is located on the lateral wall of the nasopharynx, defining and protecting the orifice of the tympanopharyngeal duct, or eustachian tube (Figure 2). Rosenmiiller's fossa is a vertical cleft, a potential space, between the posterior lip of the torus tubarius and the adenoidal pad. It is of considerable importance because many of the insidious malignancies of the pharynx have their origin in this space. The adenoid, or pharyngeal tonsil, is a primary lymph node of first line defense for inflammation involving the upper airway.
OROPHARYNX
|
The lingual tonsils are located on either side of the dorsum of the tongue anterior to the epiglottis (Figure 5). The median glossoepiglottic fold and the two lateral glossoepiglottic folds attach the epiglottis to the base of the tongue. |
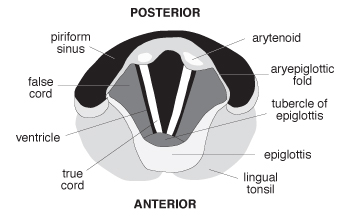 Figure 5. The larynx viewed from above and oriented as it would be seen with a fiberoptic
endoscope. Figure 5. The larynx viewed from above and oriented as it would be seen with a fiberoptic
endoscope. |
HYPOPHARYNX
The valleculae are cup shaped spaces, separated by the median glossoepiglottic fold, posterior to the base of the tongue and anterior to the epiglottis. To the right and to the left of the larynx are the piriform sinuses, gutter like structures which direct food to the esophagus.
LARYNX
The framework of the larynx is formed by the thyroid, cricoid, and epiglottic cartilages and by pairs of arytenoid, corniculate, and cuneiform cartilages. The aryepiglottic folds and the arytenoids are located immediately behind the epiglottis (Figure 5). The aperture of the glottis (rima glottidis) is formed by the true vocal cords (vocal folds; plicae vocales) and the posterior commissure between the arytenoids. The anterior ligament of the true vocal cords is located at the anterior angle of the vocal cords. Between the true vocal cords and the false vocal cords (vestibular folds; plicae ventriculares) is the laryngeal ventricle. The nodular swellings located medially in the aryepiglottic folds are the corniculate cartilages which sit on top of the arytenoid cartilages. Lateral to the corniculate cartilages are the cuneiform cartilages.
The true vocal cords are anteriorly attached to the thyroid cartilage. The posterior attachment is to the vocal processes of the arytenoid cartilages. The true, cords often reflect light in such a manner that they appear whiter than the surrounding mucosa. The strong vocal ligaments are covered by connective tissue and a thin layer of epithelium. Reinke's space is the potential space between the vocal ligaments and the subepithelial connective tissue layer. The mobile arytenoid cartilages move in and out with respiration and phonation.
THE PARANASAL SINUSES
|
Thin bony partitions separate the sinus cavities from other structures of the head. The frontal, ethmoid, and maxillary sinuses comprise the three walls of the orbit. The sella turcica is superior to the sphenoid sinus; other adjacent structures include the internal carotid artery, the optic nerve, and the brain. The frontal sinus is also juxtaposed to the brain; infection could extend posteriorly into the dura and brain, inferiorly into the orbit, or anteriorly into bone and periosteum, resulting in a Pott's puffy tumor. The maxillary sinuses (antra of Highmore) are the largest of the paranasal sinuses (Figure 6). The alveolar processes of the upper dentition often extend into the floor of the maxillary sinus. The ostium draining the sinus is located superiorly on the posterior medial wall of the sinus; accessory sinus ostia are not uncommonly found. Ciliary action sweeps secretions and bacteria against the force of gravity up to the small ostium and out into the middle meatus. |
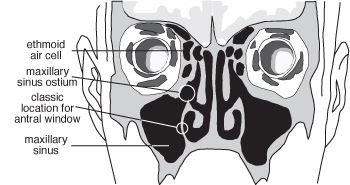 Figure 6. A frontal section of the head. In this section, eight ethmoidal air cells
(four on each side) are shown in their location medial to the orbits. Note that the
ethmoid labyrinth extends above the level of the cribriform plate. A rather large
maxillary sinus ostium is demonstrated, as well as the location in the inferior meatus
for surgical placement of antral windows. Figure 6. A frontal section of the head. In this section, eight ethmoidal air cells
(four on each side) are shown in their location medial to the orbits. Note that the
ethmoid labyrinth extends above the level of the cribriform plate. A rather large
maxillary sinus ostium is demonstrated, as well as the location in the inferior meatus
for surgical placement of antral windows. |
|
From three to twelve ethmoid air cells comprise each side of the delicate ethmoid labyrinth, located along the medial wall of each orbit (Figures 6 and 7). Those which have ostia emptying into the middle meatus are defmed as anterior ethmoid cells and those that have ostia that empty into the superior or supreme meatus are defined as posterior. A few air cells which might drain in or superior to the ethmoid bulla would be designated by some anatomists as middle ethmoidal air cells. Posterior ethmoid sinuses may also drain into the sphenoid sinus. The fovea ethmoidalis, the roof of the ethmoid sinuses, extends above the level of the cribriform plate. The ethmoid labyrinth is separated from the orbit by the lamina papyracea (lamina orbitalis ossis ethmoidalis). The middle ethmoid air cells medially form the prominent bulge in the middle meatus called the ethmoid bulla (bulla ethmoidalis ossis ethmoidalis; ethmoid antrum). On occasion, a misplaced posterior ethmoid cell will locate in the middle turbinate, forming a concha bullosa. Anterior ethmoid cells may be found in the agger nasi and uncinate process. Ethmoid cells which have migrated into the superior roof of the maxillary sinuses are called Haller cells. |
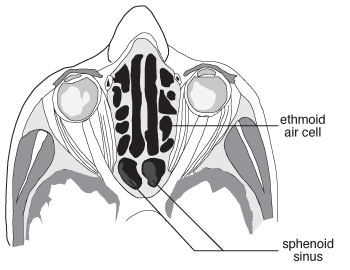 Figure 7. A horizontal section through the head at the level of the orbits and the
sphenoid and ethmoid sinuses. Figure 7. A horizontal section through the head at the level of the orbits and the
sphenoid and ethmoid sinuses. |
The sphenoid sinus is a posterior extension of the ethmoid labyrinth (Figures 4 and 7). It is centrally placed in the skull, and pain originating from the sinus may be referred behind the eyes, to the temples, or to the occiput. An irregular bony septum forms two or more often asymmetrical structures. Each portion of the sphenoid sinus empties into the sphenoethmoidal recess via an ostium in its superior anterior wall.
If the ethmoid labyrinth is followed anteriorly and superiorly, it is evident that the frontal sinus (Figure 4), like the sphenoid sinus, is actually an enlarged, septated ethmoid air cell. The extent of the frontal sinus is variable. Some individuals have only a rudimentary frontal sinus; in others, the sinus may be so large that it extends out over the orbit or almost back to the temporal bone. A large frontal sinus causes the frontal bossing characteristic of some individuals. The frontal sinus drains to the middle meatus via the nasofrontal duct.
NASAL INNERVATION
|
The olfactory epithelium is located on the nasal roof. Nerve fibers from the olfactory cells penetrate the cribriform plate and enter the olfactory bulb of the brain. The other sensory nerves are largely derived from the ophthalmic and maxillary divisions of the trigeminal (V) nerve (Figure 8). The anterior and posterior ethmoid nerves and the infratrochlear nerve are branches of the ophthalmic nerve. The anterior ethmoid nerve enters through a small foramen in the anterior vault of the nose; branches innervate the anterior septum, the anterior lateral wall, and a portion of the external nose. Branches of the maxillary division of the trigeminal nerve originate in the pterygopalatine ganglion and enter the nasal cavity through the sphenopalatine foramen in the pterygopalatine fossa. The nasopalatine nerve innervates the middle and posterior septum and terminates in the incisive canal. The posterior lateral branches of the palatine nerve innervate the turbinates and meati, and the anterior superior alveolar branch of the infraorbital nerve innervates the nasal floor and the anterior portion of the inferior meatus, and the maxillary sinus. The pharyngeal nerve innervates the sphenoid sinus and the nasopharynx. A few other small sensory branches pass from the mandibular division of the fifth nerve up through the naris into the vestibule of the nose; in the nose these form a network of nerves. |
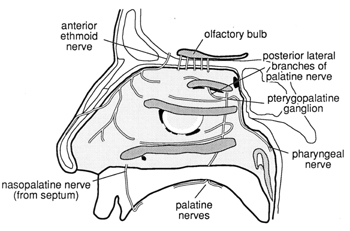 Figure 8. Innervation of the lateral nasal wall. The anterior ethmoid nerve is a branch
of the ophthalmic division of the trigeminal nerve. Branches of the maxillary division
of the trigeminal nerve originate in the pterygopalatine ganglion. Figure 8. Innervation of the lateral nasal wall. The anterior ethmoid nerve is a branch
of the ophthalmic division of the trigeminal nerve. Branches of the maxillary division
of the trigeminal nerve originate in the pterygopalatine ganglion. |
When anesthetizing the nose, it is only important to place anesthesia in the anterior vault of the nose, posterior to the inferior and middle turbinates, and in the area of the anterior septum. Anesthesia of the pharynx and larynx is not required for routine fiberoptic examination of the upper airway.
In memoriam, John Canty Selner, MD (1936-2006)