Continuous Quality Improvement is a key value of the Department of Medicine and the Internal Medicine Residency Program. Our curriculum involves all levels of residents and prepares them to critically evaluate hospital processes, identify system errors and implement potential system improvements that ensure patient safety. Residents are empowered to make positive change.
The making healthcare SAFER (MHCS) course
Course designed to decrease preventable medical errors, improve quality of healthcare, and promote teamwork in an inter-specialty, inter-professional manner during orientation.
2018 focus: best practices for infection prevention, quality and teamwork in healthcare delivery
2019 focus: integrating asepsis into daily hospital activities and safety awareness. Interns participated in stations to address asepsis techniques and reinforcement of concepts of handwashing repetition. They also joined in a safety simulation to measure the participant’s ability to identify patient safety concerns. Interns learned how to report and remediate these concerns by reporting on the Safety online system.
Making Central Lines SAFER course
Initial knowledge based course followed by a cadaver-based competency in the fall. Residents who have successfully completed both courses may place central lines under direct supervision until deemed competent for procedure credentialing privileges.

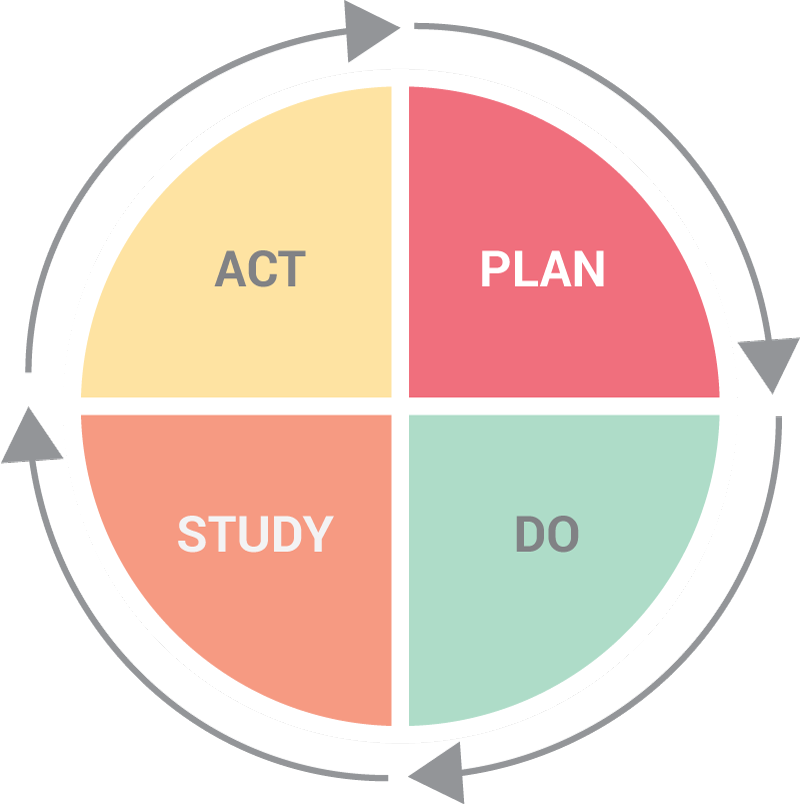
Curriculum on continuous quality improvement:
Attend at Morbidity, Mortality, and continuous quality Improvement
Participation and engagement in multi-disciplinary unit based and departmental based quality committees
Regular notification and initiatives of hospital-wide “report card” showing rates of catheter-associated urinary tract infections (CAUTI), central line associated bloodstream infection (CLABSI), and ventilator associated pneumonia (VAP).
Involvement in the AU Health Quality Improvement Symposium.