Hospitals in rural Georgia are limited in their ability to care for patients with emergency conditions due to a lack of resources and as a result patient in rural areas often experience poorer health outcomes for the same conditions than residents in suburban and urban areas of our state.
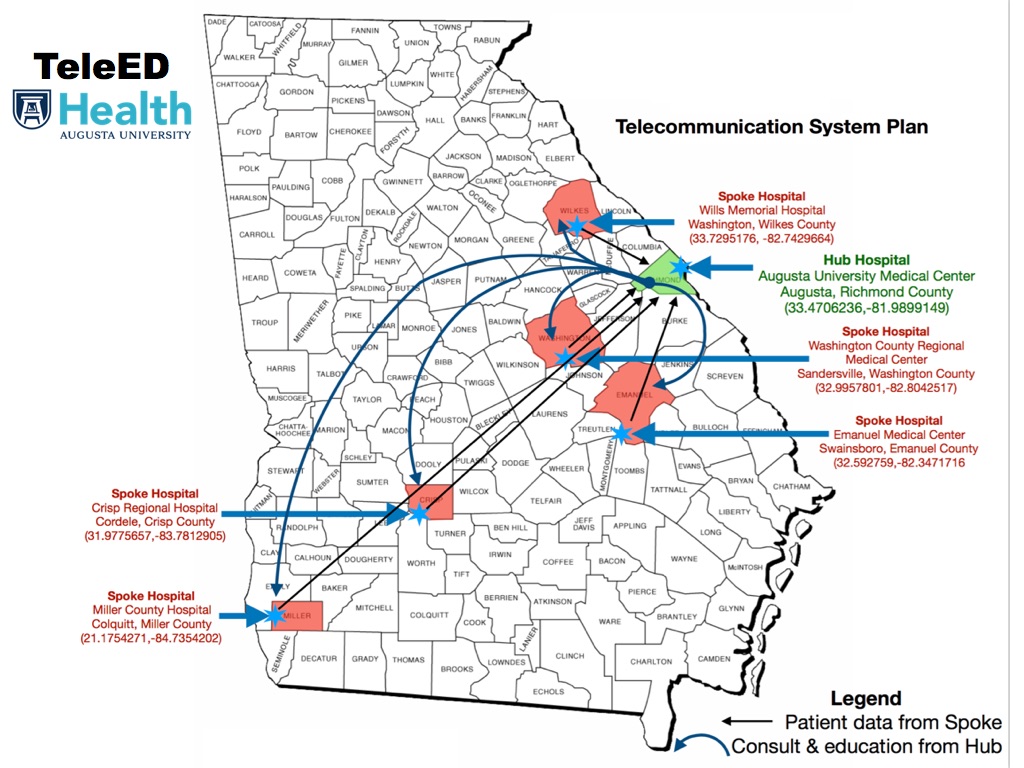
The challenge is how to provide the same level of emergency care in rural areas as in suburban and urban areas. Our solution is through the use of telemedicine, specifically the Tele-Emergency Department (TeleED) program at AUMC. The TeleED program aims to provide specialized emergency medicine care in these rural communities using a telemedicine spoke and hub model, in order to meet national quality of care standards in rural emergency departments, eliminate unnecessary patient transfers from rural hospitals while decreasing the cost of care and improving the revenue potential in rural hospitals.
The TeleED program is funded through a USDA grant and initiated October 2019 with 5 spoke hospitals: Wills Memorial Hospital (Washington GA), Washington County Regional Medical Center (Sandersville, GA), Emanuel Medical Center (Swainsboro, GA), Crisp Regional Health Services (Cordele, GA), and Hospital Authority of Miller County (Colquitt, GA). Augusta University Medical Center in Augusta Georgia, serves as the Hub site with the TeleED program as a part of a comprehensive telemedicine program.
In 2002, faculty from the departments of Neurology and Emergency Medicine at the Medical College of Georgia / Augusta University (MCG/Augusta University) collaborated to facilitate acute stroke management in rural EDs and developed a tool to assist physicians in those EDs in identifying to which patients tissue Plasminogen Activator (tPA) should be offered. The result was REACH (Remote Evaluation of Acute isCHemic stroke), a simple Internet based system which is wireless on either end with video capability to see and examine the patient in the remote ED and perform an NIH stroke assessment, as well as view the patient’s CT scan. The patient’s family could be given accurate information about the risks and benefits of thrombolytic therapy. tPA could be administered right in the rural ED, enabling the patient to be transferred leisurely and safely, now that time sensitive assessments and treatment options had been addressed. The system is staffed 24/7/365 by rotating faculty neurologists and one EM attending.
In order to meet a request from the New York State Health Department to build a telestroke network in their state in 2006, a company, REACH Call, Inc (now REACH Health) was created. Some 20 hubs and spokes in the MCG/Augusta University hub and spoke network cover much of the state using the REACH system. Additionally, Georgia has a second hub at St. Joseph’s/Candler in Savannah with 9 spokes of its own which are REACH based. And a third REACH network is used by Piedmont Hospitals in the Atlanta area. Other states have one or more hubs and spokes in place including South Carolina, Florida, Louisiana, Ohio, Pennsylvania, Michigan, New Jersey, New York, Massachusetts, and Illinois. All this makes the REACH system the busiest stroke network in the US Stroke Belt and among the oldest, busiest, and most prolific in the world.
Since its humble beginnings, MCG/Augusta University has grown to be the hub for some 30 spoke hospitals, from within the same county to over 200 miles away and across the state line into South Carolina with more Georgia and SC sites already slated to start up in the upcoming months. Additionally, the faculty of the MCG/Augusta University system now cover call for the entire Savannah network 24/7/365.
 Member hospitals include:
Member hospitals include:
Well over 3600 consultations have been performed in our network alone and tPA has been given more than 700 times, right at 20% which is comparable to only a few national leading center’s on-site treatment. Complications from hemorrhage rate has been under the national average at 2.5% and bleeds have been minor, making it clear that treating patients via telemedicine is as safe as treating in-house. Not only is it safe, but patients treated via REACH are treated 20 minutes faster than the national average at major centers around the country.
Our REACH group has learned much as we have expanded the program: